
Loading...

Loading...
2025-06-27
Antara
Non-verbal communication helps create meaningful connections with dementia patients. Words often fail these patients, and alternative methods become essential. Research reveals a concerning trend - people with dementia spend only a few minutes of their day in social interactions. They spend most of their time without any activity. This isolation creates significant problems.
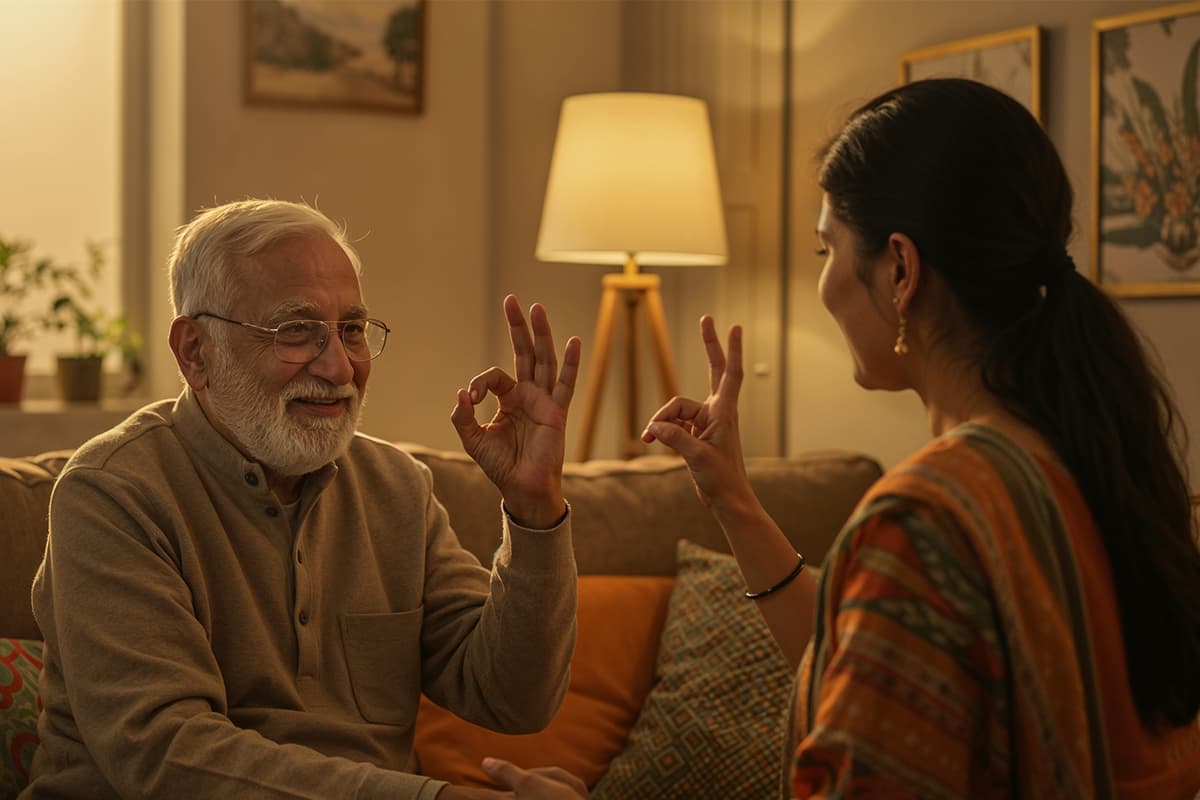
People living with dementia face depression, anxiety, and feelings of neglect due to communication barriers. These challenges make them confused and angry. Caregivers struggle to understand their loved one's needs because of these issues. Research points to six non-verbal strategies that bridge this communication gap. These strategies include:
Patients naturally focus on tone, body language, and facial expressions as their verbal abilities decline. They try to make sense of interactions through these non-verbal cues. Visual aids provide alternative ways to maintain connections in dementia care. This piece shows practical techniques that restore dignity and understanding between caregivers and patients.
People with dementia lose their ability to understand language and speak fluently as the condition progresses. Their non-verbal communication skills often stay intact remarkably. This preservation creates a vital pathway to connect when words become harder to use.
Research shows a strong link between problems in non-verbal communication and lower quality of life for people with dementia. Studies also show these problems are directly associated with increased neuropsychiatric symptoms and higher caregiver burden. Knowing how to communicate non-verbally becomes more important than verbal skills if you have moderate to severe dementia.
Care settings demonstrate the value of non-verbal approaches clearly. People with dementia who find verbal expression difficult may become frustrated, anxious, or withdrawn. They often use other methods to express their needs and emotions:
Non-verbal communication helps beyond simple interaction. Tactile communication—like holding hands—provides comfort and reduces agitation especially when you have sensory impairments along with dementia. Art therapy, drawing, and music let people express feelings without using words.
Visual aids displayed on tablets and computers boost these approaches. Simple images help patients point to their needs or priorities, which eliminates the frustration of searching for words they can't find.
Non-verbal techniques help care partners recognise and meet needs that might otherwise stay unexpressed. This understanding prevents misreading of intentions that could lead to increased agitation or aggression. Yes, it is true that training caregivers in non-verbal communication skills substantially improves dementia patients' quality of life in care settings of all types.
People with dementia understand body language better than words. Studies show that non-verbal elements make up communication in dementia people. Body language accounts for the majority, voice tone takes up the next part, and word contribution is minimal. This explains why people with dementia can understand feelings better than spoken words.
You can build powerful connections through facial expressions. A warm smile or raised eyebrow speaks happiness or curiosity better than words. Good eye contact builds trust, and you show respect by sitting or kneeling at eye level instead of standing over someone, which might seem threatening.
Touch becomes more important as verbal skills decline. Simple gestures like holding hands, giving soft back rubs, or patting shoulders can comfort and reassure. Research shows that a five-minute hand massage can lower cortisol levels and help people relax. Scientists also found that daily foot massages over two weeks reduced agitation, and these positive effects lasted for weeks.
Visual aids work well to bridge communication gaps. These include:
These tools help people share more factual information during conversations while reducing unclear or repetitive statements. People with dementia also take turns better and stay on topic more often.
Your environment affects communication success a lot. A quiet space away from TV or radio noise helps, and good lighting reduces confusing shadows. Take a deep breath to calm yourself before any interaction. This shows calmness through mirroring—where people naturally match each other's emotional states.
Regular use of the same visual aids strengthens understanding and recognition. Most importantly, treating people with dignity never gets old—even in advanced stages, people with dementia still feel emotions and recognise a caring presence.
Communicating with dementia patients needs nowhere near just words. Non-verbal techniques build powerful bridges when language skills fade. Eye contact, facial expressions, gentle touch, and visual aids create pathways to understanding that stay open even in advanced stages.
Research shows that people with dementia keep their ability to recognise caring gestures and emotional tones, even as their verbal skills decline. These lasting connections allow meaningful bonds to continue through cognitive changes. Caregivers who become skilled at these alternative methods see amazing improvements in their patient's well-being.
These approaches give back dignity to those who don't deal very well with expression. Non-verbal techniques celebrate what people can still do instead of focusing on what's lost. Both care partners can build deeper connections with less frustration.
Small changes can make big differences. Quiet spaces, consistent visual aids, and mindful body language help create better interactions. Each person deserves treatment as a complete human being - not just someone with an illness. This approach opens up real understanding between people.
Studies show that dementia patients receive the majority of information through non-verbal gestures. These techniques have proven to work:
Body language plays a crucial role in dementia care. Non-verbal elements (body language or tone of your voice) make up most of the communication. This explains why people with dementia often understand emotional meaning better than words.
People with dementia notice negative body language like sighs or raised eyebrows quickly. Crossed arms can seem unfriendly, but an open, inviting posture shows you care. As speaking becomes harder, patients pay more attention to these non-verbal signs to understand intentions.
Visual communication methods boost understanding a lot. Memory books, reminder cards, and communication boards help with recalling and finding words. Tools like Talking Mats—picture sets with text captions—help conversations about needs and priorities. Hospitals use simple visual markers like blue flower symbols. These help the core team spot dementia patients and adjust care. Visual prompts on tablets or computers let patients point to what they want, which boosts appetite and involvement.
Touch works like a universal language to bring out positive behaviours. Research shows five minutes of hand massage lowers cortisol levels and helps people relax. At Antara memory care, staff knows all ways to use touch especially for dementia patients. They are experts at safe approaches include gentle hand-holding, shoulder touches, and hugs—when appropriate. Watch body language to ensure comfort since someone's comfort with touch can change. Before giving hands-on care, tell them what you plan to do: "I'm going to put lotion on your feet. Does that feel okay?"
Non-verbal communication works best alongside speech. Even when words don't make sense, a kind tone, warm smile, and caring touch get the message across. Think about it like talking to someone who speaks a different language—mix words with actions that show what you mean.
Non-verbal approaches become extra valuable for people who have sensory problems along with dementia. People in the late stages still benefit from hearing familiar voices, even if they can't answer. The best approach uses both verbal and non-verbal methods, changing the mix as needs shift.

Please fill in the form and submit the details to request an appointment.